We seek residents who are driven to advance the field of Neurology. Our program balances breadth and depth in clinical training with an extensive didactic and problem-based learning curriculum.
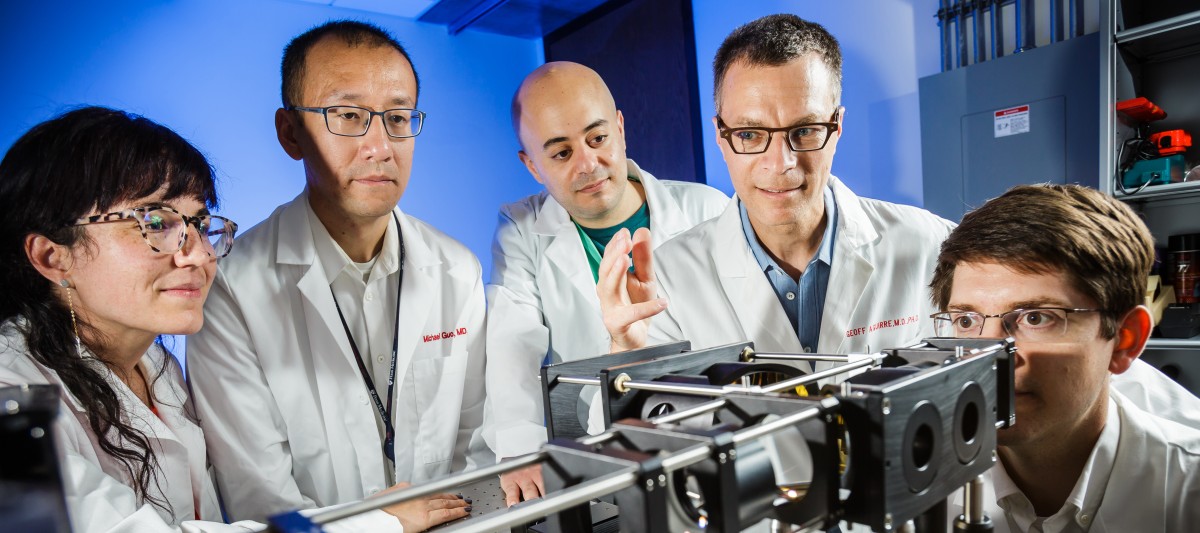
Residents benefit from an integrated career development curriculum and an array of academic career electives in Research, Education, Health Equities, Global Health, and Health Care Leadership and Quality Improvement. The Department holds an NINDS R25 grant, which allows research-oriented residents to apply for additional laboratory time during residency.

Residents dedicated to other, non-laboratory scholarly activities can also receive additional elective time during residency. We are committed to supporting our trainees through their transition to career independence.
We are located on the historic campus of the University of Pennsylvania, home of the Nation’s first medical school. The geographic integration of the University of Pennsylvania allows our trainees to access the extraordinary academic resources of the larger University as part of their scholarly and career development.
Most of our residents live in downtown Philadelphia, within walking and biking distance of campus. The vibrant cultural, athletic, dining, and social scene of Philadelphia provides the backdrop for friendships that extend well beyond the halls of the hospital.
Our department is one the largest of its kind, with over 100 full-time faculty distributed over 12 clinical divisions and 20 sub-speciality programs. Most of our faculty are engaged in academic pursuits, in addition to their clinical work. Clinical training is principally at the Hospital of the University of Pennsylvania, the flagship hospital of the Penn Health System, and one of the Nation’s top hospitals.
The four other sites of training are located in downtown Philadelphia within walking or biking distance. The Children’s Hospital of Philadelphia (CHOP), consistently ranked as the top hospital of its kind, is the site of training in pediatric neurology. The Penn Presbyterian Medical Center is the integrated site of trauma care for the health system, and provides additional training in neuro-critical care. The Philadelphia Veterans Association Medical Center (VAMC) provides an experience caring for our veterans in our region in several outpatient sub-specialties. Pennsylvania Hospital (founded 1751) is the Nation’s first hospital and is the home of the Parkinson Disease and Movement Disorders Center, and the Penn Comprehensive ALS Center.
Program details and application information are available in the Apply page.
If you are interested in the Fellowship Programs in Neurology, please visit our dedicated page.